photo by Petr Kratochvil (click image for more)
Many of my headache patients come to see me and describe their intense headaches as “migraines.” This self diagnosis is purely based on the high level of discomfort they are experiencing.
Fortunately, most headaches are not migraines, even the very intense ones. And knowing what type of headache you have is crucial in determining what course of action will cure you.
According to the American Headache Society, over 78% of people will suffer tension type headaches during their lifetime. A much smaller percentage will ever have a true migraine. Therefore, if you have intense headaches, instead of self diagnosing yourself, go see your chiropractor or family doctor for a professional opinion. Having treated headache patients for over 10 years and having taught a headache class at the University of Victoria, I am well aware of sufferers and their tendency towards self-diagnosis. If the self diagnosis is wrong it can stop them from getting to the pain free stages they so desire because they are doing the wrong things.
This post is not meant to replace diagnosis by a professional, but to help you see that you may have wrongly self diagnosed and therefore are on the wrong track.
WHAT CAUSES MIGRAINES AND TENSION TYPE HEADACHES?
 If you were to drill a hole through each of your cheek bones (front to back) within about 2 inches you would hit a bundle of nerves known as the trigeminal ganglion. This is a squid-like branch of nerves that connect to the eyes, forehead, scalp, face, jaw and temple region and then relays them all back to the spinal chord. In the spinal chord the trigeminal nerves connect to the neck nerves via an area called the trigemino-cervical nucleus. The trigeminal ganglion is involved in both migraines and tension type headaches but only tension type headaches affect the trigemino-cervical nerves. The following information will teach you some basics to differentiate migraines from tension headaches.
If you were to drill a hole through each of your cheek bones (front to back) within about 2 inches you would hit a bundle of nerves known as the trigeminal ganglion. This is a squid-like branch of nerves that connect to the eyes, forehead, scalp, face, jaw and temple region and then relays them all back to the spinal chord. In the spinal chord the trigeminal nerves connect to the neck nerves via an area called the trigemino-cervical nucleus. The trigeminal ganglion is involved in both migraines and tension type headaches but only tension type headaches affect the trigemino-cervical nerves. The following information will teach you some basics to differentiate migraines from tension headaches.
MIGRAINES
Because the trigeminal nerves interact with blood vessels the foods we eat can trigger migraine headaches. Migraines are therefore different from tension type headaches because they can be triggered by wine, cheese, chocolate or caffeine. Migraines also don’t involve the neck or back of the head and are usually around the temple and eye area on one side only. The pain is typically a throbbing or pulsing sensation.
photo by Petr Kratochvil (click image for more)
Migraines typically occur only a couple of times per month and last minutes to hours but generally not days. Further, if just before you feel the headache you have visual disturbances or light and sound hypersensitivity, this points towards migraines. The typical migraine patient has migraines in their family history and has had migraines since adolescence. Typically, migraines do not respond much to ibuprofen, tylenol or aspirin. Women are more prone then men to migraines. See your chiropractor to determine if you are indeed suffering from migraines and receive the appropriate nutritional advice and treatments.
TENSION TYPE HEADACHES
The tension type headache patient usually has neck pain before their headaches. Classic tension headaches affect the rim of your scalp like a sweat band (i.e.: forehead, sides of the head and back of the head) and both sides are affected equally. Unlike migraines, tension headaches can last more than an hour and can even be constant for 2 or more days. Tylenol, ibuprofen and aspirin generally are quite helpful at reducing tension headaches. Tension headaches typically manifest several times per week and feel like constant pressure or pain — they do not pulse like migraines. No pre-headache visual or hearing issues occur with tension headaches.
Tension type headaches involve the cervical nerves and migraines do not. This is why neck injury from muscle or joint trauma or prolonged bad posture is usually the sole cause of tension headaches. They affect the neck nerves which communicate with the trigeminal ganglion which in turn sends nerves to the scalp and face, therefore causing the head pain associated with headaches. Sometimes tension type headaches are more severe than even true migraines, leading the sufferer to re-label it a “migraine.”
Because the neck causes all or most of the head and face symptoms for tension type headaches, treating the muscles and joints of the neck is usually the solution to years of suffering. People don’t know their neck is causing their debilitating headaches. At our clinic we’ve developed a series of treatments that are very effective at dealing with tension headaches.
Even long term, well entrenched tension type headaches can be cured. Our clinic also has designed a 10 week exercise rehabilitation and manual therapy program to solve even the longest term headaches. As an example, one of our headache patients let us do a documentary on her full recovery after 13 years of debilitating headaches. Please take the time to watch:
CLICK IMAGE TO SEE VIDEO
Some patients have symptoms of both tension headaches and migraines. Sometimes, these patients receive treatment for their tension headaches and their migraines disappear. This is because both types of headaches affect the trigeminal ganglion. Therefore, in some patients, tension headaches trigger the migraines. So if you remove the tension headache, you remove the migraine by default.
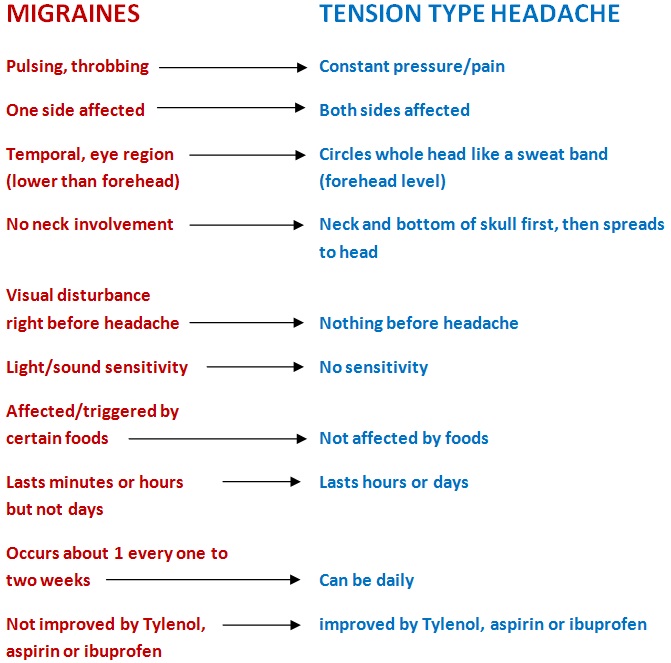
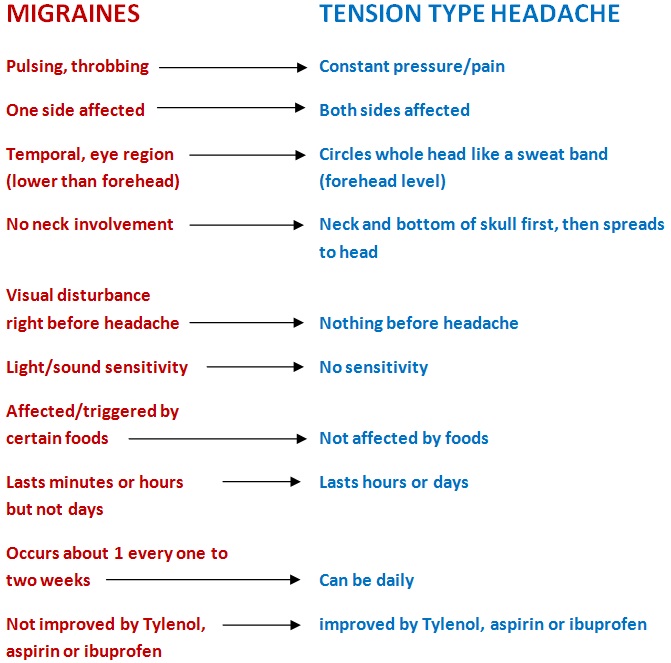
To recap the difference between tension headaches and migraines, see the diagram below for an easy comparison:
Please do not use this post as substitute for professional diagnosis. There are many other types of headaches such as cluster headaches, temporal arteritis, toxic headaches and others that mimic certain aspects of migraines and tension headaches. A clinician such as your chiropractor or family doctor will be able to differentiate from these and give you a sure diagnosis.